Using HIV immunotherapy, scientists from the University of Pittsburgh Graduate School of Public Health have made an interesting development in the race for a cure. While “cure” is a strong and coveted word in the field of medicine, what they’ve discovered comes pretty close.
So what is all the hype surrounding this revolutionary immunotherapy and how did scientists discover it?
Let’s take a look.
This powerful all-in-one immunotherapy is designed to kick HIV out of hiding from the body’s DNA within the immune system. Not only does it find it – it kills it. The “kick and kill” strategy has been around for awhile now, and this promising therapy is the highest on the list because it not only brings the HIV cells out of hiding, but it also recruits healthy cells to help kill the virus.
In the laboratory, scientists used existing cells from HIV patients to find the actual cells that are harboring the HIV.
Antiretroviral Therapy (ART)
Antiretroviral therapy (ART) is the first in line for current treatment. It controls HIV so well that it practically keeps the virus completely hidden in the blood. While this is great because it lowers the risk of contagion, the HIV is still very much there. It’s just in a dormant state, hiding within T helper cells of the human body.
Also, there is a long list of side effects from ART.
These include gastrointestinal and cardiovascular complications, bleeding, and even insulin resistance. The therapy also potentially compromises bone density and health of the liver.
But with the new immunotherapy on the horizon, ART may become obsolete.
So How Does HIV Immunotherapy Work?
The immune system is very busy controlling a virus that is prevalent in over 95% of HIV patients. Scientists call this Cytomegalovirus (CMV). Scientists realized that maybe they could study the cells that fight CMV and see if they could activate CMV- specific T helper cells.
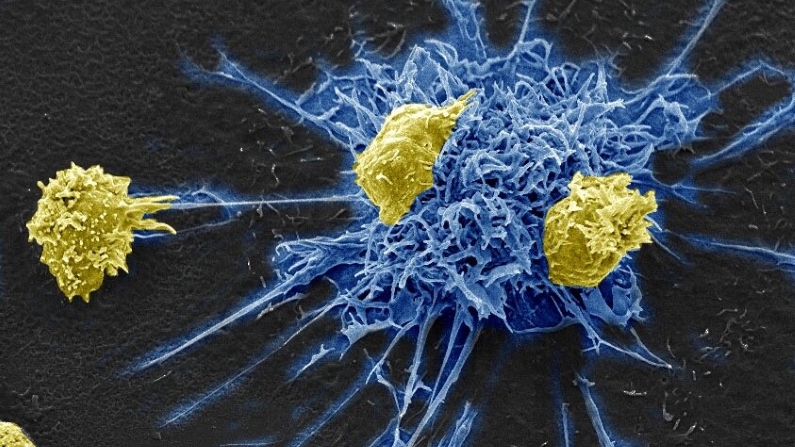
Along with targeting the discovery of these T helper cells, scientist Mailliard from the University of Pittsburgh also wanted to isolate dendritic cells.
Dendritic cells are critical in assigning roles to its other immune counterparts and thus, are essential for HIV immunotherapies.
By using antigen-presenting type 1-polarized, monocyte-derived dendritic cells (MDC1), we are able to find and activate CMV-specific T helper cells.
And once we activated them, the true experiment began.
According to Mailliard, “Without adding any other drug or therapy, MDC1 were then able to recruit killer T cells to eliminate the virally infected cells. With just MDC1, we achieved both kick and kill. To our knowledge, this is the first study to program dendritic cells to incorporate CMV to get the kick, and also to get the kill.”
The University of Pittsburgh is now pursuing funding for real clinical trials to begin testing in humans.

What Could This Mean for the Field of HIV Medicine?
It means that these findings may lead to an impactful vaccine; one that would allow people living with HIV to stop taking ART every day.
It also opens the door for a cure, as opposed to just a better quality of life that ART gives. The retrovirus therapy allows HIV patients to live a more peaceful life, without symptoms constantly flaring up – it leaves the virus virtually quiet within the blood.
But the immunotherapy utilizing MDC1 and T helper cells actually kills HIV cells. With more research and human clinical trials, this could certainly lead to actually fighting the powerful disease and destroying HIV altogether.
For more knowledge about living with HIV and the race for a cure, visit https://www.hiv.gov/hiv-basics.